IN THIS ISSUE: FACLP Awards | Webb Fellowship Awards | CLP 2024 Posters | BOPs | What's on the Web | A&E Abstracts
Another random selection from...
More Top-Scoring Posters at CLP 2024
From a record number of submissions
A record number of submissions for both posters and oral papers this year resulted in more than 450 poster abstracts and 119 brief oral paper abstracts reviewed for CLP 2024. Here is a selection of top-scoring trainee submissions—highlighting early-career presenters—in six of the most-represented topic categories with comments from chair and vice-chair of the Oral Papers & Posters Subcommittee, Michael Peterson, MD, PhD, FACLP, and VaKara Meyer Karre, MD.

Michael Peterson, MD, PhD, FACLP, and VaKara Meyer Karre, MD.
The CLP 2024 poster session in Miami (Thursday, November 7, 5:30-7:30 PM) will showcase 233 posters—the largest number ever at an ACLP Annual Meeting—many from trainees. Be sure to attend the always exciting and interactive poster session!
More posters were featured in the last issue of ACLP New here.
COLLABORATIVE AND INTEGRATED CARE
Nourishing the Golden Years: Understanding and Managing Anorexia of Aging
Lead presenter: Eslam Elhossieny, MBBCh.

Eslam Elhossieny, MBBCh
Our relationship with food endures a variety of changes during our lifetime. The term Anorexia of Aging (AoA) indicates multifactorial reduction in appetite, regulation of food intake in the elderly, even in healthy elderly populations with adequate food sources available.
AoA is influenced by various factors including but not limited to the aging process. The reported prevalence of AoA ranges from up to 25% in home dwellers to 62% in hospital populations, and 85% in nursing home populations (Cox, et al., 2019).
In hospital settings, the often-overlooked issue of AoA triggers unwarranted polypharmacy with appetite boosting medications and oftentimes results in psychiatric consultation. The absence of a systematic, stepwise approach within C-L Psychiatry potentially can lead to unguided interventions, say the presenters. The insufficiency of current strategies is evident (Megha Mulchandani, et al., 2021), necessitating a focused and interdisciplinary collaboration between C-L Psychiatry, Geriatric Medicine, and Nutritionists.
Overall, findings suggest a need for developing a stepwise collaborative multidisciplinary approach in the elderly population for identifying risk factors for malnutrition that includes clinical, socioeconomic, physiological, psychological, and environmental factors.
The presenters are developing a screening tool/stepwise clinical approach to help guide medical and psychiatric teams, staff members, and nutritionists to develop a personalized care plan for elderly patients with anorexia in hospital settings. A patient-centered, stepwise approach to managing anorexia in hospitalized older adults can optimize care, decrease polypharmacy, and emphasize patients’ overall well-being, say the presenters.

The presenting team (l-r): Gerard Casale, MD, MBBCh, Eslam Elhossieny, MBBCh, and Shruti Tiwari, MD.
DIVERSITY, EQUITY AND INCLUSION
Promoting Equity in Behavioral Emergency Management: A Pilot Program Utilizing the Pittsburgh Agitation Scale for Addressing Racial Disparities
Lead presenter: Brandon Rivera.

Brandon Rivera
Behavioral Emergency Incidents (BEIs) present challenges for hospitals, often leading to resource-intensive interventions and delayed discharge. Racial disparities in BEI management are well-documented, with Black patients experiencing higher rates of incidents, restraints, and security involvement compared to their White counterparts.
The presenters conducted a retrospective study to assess if minority patients were disproportionately affected by BEIs necessitating security presence and restraint use. They found that Black patients were 1.5 times more likely to experience a BEI compared to Whites and 2.5 times more likely compared to other ethnic groups. Additionally, Black patients with a behavioral response code had significantly higher rates of physical restraint usage compared to Whites (32.3% vs. 12.8%, p=0.0037).
Findings underscore the necessity for objective assessment tools. implementation of the Pittsburgh Agitation Scale (PAS) is recommended, a validated and evidence-based tool for predicting violence. PAS efficiently evaluates agitation severity across four dimensions, taking into account factors that are unrelated to race.
The presenters’ hypothesis suggests that this proactive approach will diminish the subjectivity inherent in restraint decisions and effectively manage patient behavior before it reaches a point where restraints and PRN [pro re nata, when required] medications are deemed necessary.
A pilot program is slated for introduction on a general adult hospital floor where behavioral emergency incidents occur frequently. Nursing staff administer PAS during each shift. Noteworthy scores trigger immediate automatic consultation with psychiatry providers for further assessment and management.
This project has the potential to alleviate racial bias in the management of behavioral emergency incidents and foster equitable care for all patients, say the presenters.
Dr. Peterson: “Interventions to prevent and manage behavioral emergencies are a critical part of C-L practice, both in emergency department and Inpatient settings. As the authors note, racial disparities in response and outcomes to BEIs are substantial, pervasive, and serious. Objective and quantitative tools can hopefully help to remove some of the biases in BEI response, and this study presents intriguing data piloting such a scale. Continuing to critically evaluate current practices and implement novel tools can hopefully help us move beyond inequities and provide better care.”
OBESITY, NUTRITION, AND EATING DISORDERS
Rapid Onset Antipsychotic-Induced Diabetes and the Role of Semaglutide: Case Report, Literature Review, and Protocol Development
Lead presenter: Reile Slattery, MD

Reile Slattery, MD
Semaglutide has been demonstrated to facilitate achieving glycemic goals and reduce risk of major adverse cardiovascular events in individuals with type 2 diabetes (T2D). Individuals with serious mental illness (SMI) experience increased rates of metabolic syndrome and associated poor outcomes compared to the general population, in part due to antipsychotic-induced weight gain (AIWG).
Here presenters report a case of rapid onset AIWG, diabetes, and hyperlipidemia, prompting them to review the literature and develop a guideline for initiation and administration of semaglutide in select psychiatric inpatients.
Daily and once-weekly glucagon-like peptide (GLP-1) receptor agonists have been observed to be effective in management of AIWG and hyperglycemia in individuals with T2D and SMI (Perlis, 2020). Case reports suggest that semaglutide, specifically as a weekly injection, is effective in the management of AIWG (Prasad, 2023) and T2D (Noda, 2022) in individuals with SMI. Clinical trials, including randomized-controlled trials, investigating the use of semaglutide in individuals with schizophrenia with and without diabetes are underway (De, 2023).
The presenters’ institution has since developed a protocol for inpatient initiation of weekly subcutaneous semaglutide for individuals with T2D on atypical antipsychotic medications for SMI management (Parish, 2024). Several individuals are currently being monitored on the protocol (data pending).

The presenting team (l-r), top row: Felicia Mendelsohn Curanaj, MD; and Reile Slattery, MD. Below: Jane Seley, DNP, MPH, FADCES. Not pictured: Fong Liu, MD.
Dr. Meyer Karre: “Worldwide adult obesity has more than doubled since 1990, leading to an increased risk of type 2 diabetes, heart disease, and certain cancers. The authors of this presentation highlight how individuals with serious mental illness experience increased rates of metabolic syndrome, in part due to antipsychotic medication administered to treat their mental illness. Glucagon-like peptide receptor agonists, such as semaglutide, have shown effectiveness in management of antipsychotic-induced weight gain and, given the frequency in which antipsychotic medication is prescribed, it is vital that C-L psychiatrists are familiar with GLP-1 receptor agonists and possible protocols for inpatient initiation of these medications.”
TRAINING, EDUCATION, MENTORSHIP, AND CAREER DEVELOPMENT
Teaching Triaging: Case-Based Consultation-Liaison Psychiatry Workshop for Residents
Lead presenter: Allison Rhodes, MD, MPH.

Allison Rhodes, MD, MPH
Triaging on the C-L Psychiatry service is a challenging skill to learn, but is often taught and learned informally. Two case-based medical education resources exist regarding triaging (Lescinskas, 2020; Chen, 2021), although both focus on preparing interns for internal medicine rotations and call. No education resources exist known to the presenters to train psychiatric residents in consultation triaging skills.
Preliminary analyses from the pilot study demonstrate that participants had increased comfort and confidence across all triaging domains. In the pre-workshop survey, only 58.3% of residents reported feeling very confident delineating a clear consult question, while in the post workshop survey 85.7% felt very confident.
Residents have also qualitatively reported substantial benefit from the workshop in improving both confidence and preparedness for rotating on call and on the C-L Psychiatry service, with interest in conducting and expanding upon simulation-based learning for C-L Psychiatry.
Pending final quantitative analysis at a different institution to assess generalizability of this intervention, the presenters aim to further develop this workshop to ultimately build an adoptable triaging curriculum across all psychiatry residencies.
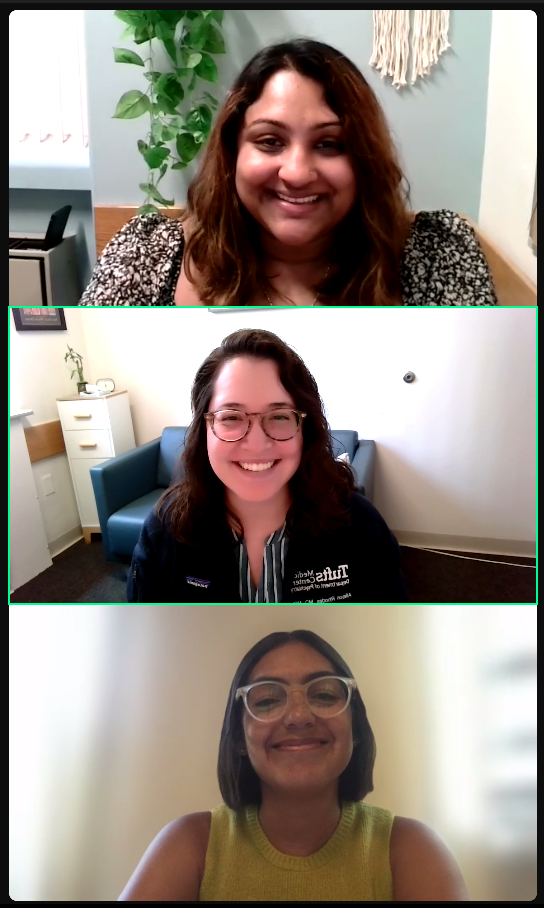
The presenting team, from top: Varsha Radhakrishnan, MD; Allison Rhodes, MD, MPH; Ashley Nieves, MD.
Dr. Peterson: “It is often skills we consider ‘core’ to the consultation-liaison service that are hardest to teach, and few shared, or validated, educational resources exist. Triaging consult requests, including defining the consult question, is one of these skills. The authors present a preliminary study of their educational workshop on triaging—with promising results in increasing learner confidence. Fortunately for academic programs, the future intent is to further validate the approach and create a shared curricular resource that other programs can also benefit from!”
NEUROCOGNITIVE DISORDERS AND NEUROPSYCHIATRY
Things are Looking Up: A Case of Progressive Supranuclear Palsy Presenting as a Car Crash
Lead presenter: Erica Bartle, MSN, PMHNP.

Erica Bartle, MSN, PMHNP
Progressive supranuclear palsy (PSP) is a rare neurodegenerative disease starting around age 65 with a prognosis of seven years and prevalence at about five in 100,000 (Globe, 2018). PSP is characterized by gait disturbances, bradykinesia, rigidity, gaze palsy, dysarthria, sleep disturbances, and cognitive impairment, with the cause of PSP unknown and treatment options limited (Bluett, 2021).
It is commonly misdiagnosed as other neurological and mood disorders, often presenting the psychiatric consultant with significant diagnostic challenges (Rowe, 2021). The presenters present a case that highlights the diagnostic complexity in an emergency setting.
PSP is a tauopathy that is easily mistaken for other conditions, including mood disorders, as early symptoms may appear psychiatric in nature (Rowe, 2021). Identifying and distinguishing between primary psychiatric illness and early symptoms of apathy and executive dysfunction in PSP are essential in accurate and timely diagnosis.
In the case study, the patient’s presenting complaint of ‘looking up’, which taken colloquially as odd, was ironically a cardinal feature of the diagnosis, but coupled with mood lability functioned as the proverbial ‘red herring’ and highlights how anchoring bias towards a psychiatric diagnosis resulted in diagnostic delay.
Barriers to accurate and timely diagnosis of PSP in emergency department settings include anchoring bias, the expectation of rapid disposition planning, and subsequent difficulties with advocating for further medical workup. Increased bias awareness, challenging assumptions, and advocacy may help improve these barriers to assist in diagnosing, treating, and disposition planning in PSP patients.

The presenting team (l-r): David Van Norstrand, MD, PhD, Erica Bartle, MSN, PMHNP, and Brittney Locke, PMHNP.
Dr. Meyer Karre: “Progressive supranuclear palsy (PSP) is a form of atypical Parkinsonian syndrome that can affect movement, gait, balance, speech, swallowing, vision, eye movements, mood, behavior, and cognition. It is an uncommon diagnosis, and its combination of psychiatric and neurologic symptoms lead to diagnostic challenges and frequent misdiagnoses. The authors of this presentation comment on barriers to timely diagnosis of PSP and highlight opportunities to raise awareness and avoid these barriers in order to provide optimal treatment to patients living with PSP.”
PSYCHOPHARMACOLOGY AND TOXICOLOGY
Use of Vitamin Supplementation for Inhalant-Induced Psychosis
Lead presenter: David Finch, MD.

David Finch, MD
Use of nitrous oxide (NO2) as a recreational dissociative agent commonly presents with neuropsychiatric symptoms mimicking first-break psychosis, leading to frequent misdiagnosis and lower efficacy treatment. A common means of inhalant intoxication, NO2 cannisters (‘whippits’) can lead to vitamin B12 deficiency secondary to the inhalant’s effects on B12’s metabolic pathway. This deficiency can present as persistent psychotic symptoms.
In a case report, the presenters demonstrate the use of intramuscular B12 supplementation for treatment of NO2-induced psychosis.
Within 24 hours of adding B12 supplementation to scheduled olanzapine, the patient exhibited clinically significant improvements in positive and negative psychosis symptoms. The patient became less disorganized, blunted, and paranoid and provided a more reliable history. After six days of B12 supplementation, the patient returned to his previous baseline, was no longer a threat to others, cared for his own needs, and demonstrated improved insight. He was discharged home to family on continued nightly olanzapine. The patient followed up with his primary care physician one week later with a continued full remission of psychiatric symptoms.
This case illustrates the need for a holistic approach to substance use disorder diagnosis and treatment, considering the significant role of nutritional etiologies in neuropsychiatric symptoms. Second-generation antipsychotics and behavioral interventions contributed to the patient’s initial safety while hospitalized, but he did not return to baseline until after receiving nutritional supplementation.
Clinicians may be tempted to discount the efficacy of nutritional supplementation in cases that do not fit classic malnutrition pictures, but integrating metabolic correction with evidence-based antipsychotic treatment proved invaluable in this case of NO2-induced B12 deficiency.
Dr. Peterson: “Presentations of secondary psychosis (e.g., not related to primary psychotic disorders such as schizophrenia) can vary widely and are due to a remarkably broad set of etiologies. Even within the subset of substance induced psychoses, variations are marked. The authors present an interesting and less common variation—with a reminder that understanding the pathophysiology can be key to appropriate treatment and recovery. In this case, vitamin supplementation was a critical element in the recovery—and an important reminder when we are evaluating future cases.”
 |
Registration for the 2024 Annual Meeting is Open!!Registration for the ACLP 2024 Annual Meeting: Promoting Whole Health through Innovative and Integrative Approaches to Consultation-Liaison Psychiatry is now open. Register here and book your accommodation at the meeting venue here. |
