IN THIS ISSUE: President's Message | Stoudemire Award | Visiting Professors | Posters | What's on the Web | A&E Abstracts
Another random selection from...
Top-Scoring Posters at CLP 2024
From a record number of submissions
A record number of submissions for both posters and oral papers this year resulted in more than 450 poster abstracts and 119 brief oral paper abstracts reviewed for CLP 2024. Here is a selection of top-scoring trainee submissions—highlighting early-career presenters—in six of the most-represented topic categories with comments from chair and vice-chair of the Oral Papers & Posters Subcommittee, Michael Peterson, MD, PhD, FACLP, and VaKara Meyer Karre, MD.

Michael Peterson, MD, PhD, FACLP, and VaKara Meyer Karre, MD.
The CLP 2024 poster session in Miami (Thursday, November 7, 5:15-7:15 PM) will showcase 233 posters—the largest number ever at an ACLP Annual Meeting—many from trainees. Be sure to attend the always exciting and interactive poster session!
*NEW this year: All posters will be 4’ x 4’.
More posters will be featured in the next issue of ACLP News.
CHILD ADOLESCENT PSYCHIATRY
A Case of Duloxetine-Induced Hypotension in a Pediatric POTS Patient
Lead presenter: Matthew Fiorillo, DO.

Matthew Fiorillo, DO
Postural Tachycardia Syndrome (POTS) is a condition characterized by tachycardia without hypotension when transitioning to the upright position. Patients present with orthostatic intolerance, and may display symptoms concerning for somatization including palpitations, light-headedness, weakness, and fatigue. Depression and anxiety are often associated with POTS, and so antidepressants are common treatment approaches. This case report involves a patient with POTS who experienced an adverse reaction to duloxetine.
Duloxetine is an inhibitor of serotonin and norepinephrine reuptake. In addition to treating depression and anxiety, the medication is well-known to have benefit in somatoform disorders. The etiology of this effect is unclear, but is likely related to the segmental and suprasegmental desensitization of neurons that is mediated by norepinephrine. This same neurotransmitter may be involved in dysautonomia. In fact, some studies have demonstrated that excess norepinephrine can exacerbate orthostatic intolerance (Schroeder, 2002). In certain subtypes of POTS, particularly those where norepinephrine is already elevated, noradrenergic medications can produce an excessive central adrenergic response (Attard, 2023). At least one case report suggests that increased synaptic norepinephrine levels can stimulate presynaptic α-2 adrenergic receptors. This, in turn, reduces norepinephrine release from nerve terminals and can lower blood pressure (Alexandrino-Silva, 2008).
This case study is important because it demonstrates that use of SNRIs or TCAs in hyperadrenergic states such as POTS can contribute to paradoxical hypotension. Antidepressants are commonly used to treat psychiatric comorbidities in POTS. Although SNRIs and TCAs can be an effective treatment in chronic pain and somatoform disorders, these medications may exacerbate POTS symptoms.
Dr. Peterson: “Somatoform disorders are a frequent reason for psychiatric consultations—in adults, adolescents, and children. A variety of syndromes— including POTS—may be poorly understood and characterized, but frequently identified in patients, and clearly have a high rate of comorbidity with somatoform disorders. Treatment approaches including cross-specialty coordination of care and psychotherapy are key, but much less is known about the role and efficacy of psychotropic medications. This case provides an interesting reaction to an SNRI in an adolescent diagnosed with POTS, and should provide a useful platform for further discussion and study of how medications may improve—or exacerbate—this condition.”
CARDIOLOGY
Can We Be Too Happy? A Variant of Broken Heart Syndrome
Lead presenter: Daniel Fisher, MD.

Daniel Fisher, MD
Happy Heart Syndrome (HHS) is a rare variant of Takotsubo cardiomyopathy (TC) associated with intense positive emotion rather than heartbreak. The presenters present a case and discuss a possible role for psychiatric consultation.
TC has been commonly referred to as the Broken Heart Syndrome. A recent review of an international registry of stress-induced cardiomyopathy cases reported that less than 5% of cases were consistent with HHS (Stiermaier, 2022). Traditionally, the pathophysiology of TC was thought to be due to a catecholamine surge from intense negative emotion (Nayeri, 2018). Now, both positive and negative emotions have been recognized.
There is a strong association between pre-existing anxiety, mood-spectrum disorders, and TC. The case study patient had no recorded history of psychiatric illness at the time of her TC diagnosis. A previous case report proposed propranolol as a preventive therapy for recurrence of traditional TC (Costin, 2011). Although this could be beneficial for both the psychiatric and physiologic components of traditional TC associated with a ‘tragic event’, a ‘happy event’ may not respond in the same way. Suppression of happiness is generally not a desirable long-term treatment. No known study has focused on the treatment of underlying psychiatric conditions in the long-term management of TC.
Patients with TC may benefit from psychiatric consultation regardless of trigger. Increased awareness and data capture for HHS may be accomplished through proactive psychiatric consultation strategies. Further study may provide insight into the pathogenesis of mood-related cardiac pathologies, provide possible preventive steps, and improve treatment outcomes.
Dr. Peterson: “Takotsubo cardiomyopathy—'broken heart syndrome'—is a classic psychosomatic medicine diagnosis, that many of us may recall from our early stages of medical training. The author of this poster summarizes advances in understanding the physiology and treatment options for this condition. The case presented is a rare variant, important for us as C-L psychiatrists to be aware of, and presents interesting questions to be answered. We love great case reports of an uncommon condition, and as the authors present, they are an important catalyst for better understanding of mechanism and treatment.”
CATATONIA
Charlson Comorbidity Index and Length of Hospitalization in Catatonia Subtypes
Lead presenter: Liliana Patarroyo Rodriguez, MD, MS

Liliana Patarroyo Rodriguez, MD, MS
The influence of medical comorbidities on catatonia outcomes remains uncertain. The presenters aimed to elucidate disparities in medical comorbidities, assessed by the Charlson Comorbidity Index (CCI), between catatonia subtypes: catatonia associated with psychiatric diagnoses (C-APD) versus catatonia due to another medical condition (C-AMC). Additionally, they investigated how these medical comorbidities impact the length of hospitalization (LOH) among catatonia subtypes.
The cohort included adults hospitalized between May 1, 2001, and May 1, 2021, diagnosed with catatonia upon admission or during hospitalization. Among the 250 patients, 245 CCI scores were accessible. Mean age was 48.3 years, 86% of the patients were white, and 55.4% were female. Of these 187 (76.3%) were diagnosed with C-APD, while 58 (23.7%) were diagnosed with C-AMC. Bush-Francis Scale mean scores were 5.4 for screening items and 11.8 for severity. The mean CCI scores were similar between patients with C-APD (2.5) and C-AMC (2.9) (p=0.34). However, patients with C-AMC had higher prevalence of previous cerebrovascular accident (p=.003) compared to those with C-APD. No significant differences were observed in other medical comorbidities. LOH was longer for patients with C-AMC compared to those with C-APD (35.6 days vs 25.6 days, p=0.002). Mean LOH did not differ (p=0.96) based on the CCI categories (mild, moderate, severe). However, when analyzing the interaction between CCI categories and catatonia subtypes, significantly longer LOH was observed among C-AMC compared to C-APD in the mild CCI category only (38.8 vs 25.4 days, p=0.049). After adjusting for the baseline CCI category, C-AMC was associated with a 1.39 times longer LOH (95% CI 1.10 to 1.77) compared to those with C-APD (p=0.006).
Data suggests that the etiology of catatonia and its comorbidity profile may influence the LOH, particularly in those with C-AMC. While C-APD was predominant, C-AMC showed a tendency towards higher comorbidities, experienced longer LOH, and had higher prevalences of stroke. Insights provided by the CCI about patient’s health status could inform clinical outcomes, emphasizing the need for evaluation and treatment of comorbid conditions, even in patients with a psychiatric etiology of catatonia.
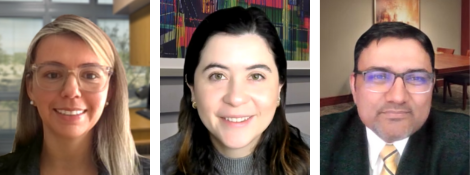
The poster team (l-r): Liliana Patarroyo-Rodriguez, MD, MS; Laura Duque, MD; and Balwinder Singh, MD, FAPA.
Dr. Peterson: “Catatonia remains a challenging diagnosis, with significant morbidity, mortality, and treatment challenges. The number of presentations annually at the ACLP reflects the ongoing efforts in the Academy to better understand and treat this condition. The authors have presented a large database of patients with catatonia, and attempt to define interactions with medical comorbidities. This is an important data set and, along with pathophysiology and treatment trials, will hopefully help us improve both diagnosis and treatment.”
PYSCHO-ONCOLOGY AND PALLIATIVE CARE
Clozapine Continuation in a Patient Requiring Chemotherapy for Lymphoma
Lead presenter: Jessica Schwartz, MD.

Jessica Schwartz, MD
Due to risk of agranulocytosis, questions remain about clozapine management in patients requiring myelosuppressive chemotherapy, even when these regimens include granulocyte colony stimulating factors to support cell counts (Barreto 2015, Rausch 2020). Clozapine dose adjustment or discontinuation to avoid agranulocytosis risks psychotic decompensation, which may limit adherence with recommended cancer treatment, especially if other medical complications arise (Grainger, 2019).
There is limited guidance regarding best practices for management of clozapine in patients requiring chemotherapy. For many patients, as in a case study presented, clozapine is integral to psychiatric symptom remission. Such remission better enables patients to engage meaningfully with recommended medical care for serious conditions including cancer and to navigate complications. While the case study patient did experience a drop in ANC with hyperCVAD, an appropriate response to filgrastim was observed and treatment was able to proceed.
The case report suggests that clozapine may be continued during chemotherapy with close clinical and laboratory monitoring. C-L psychiatrists serve an important role in advocating for patients to continue clozapine treatment in the interest of ongoing psychiatric symptom stability and quality of life, especially when faced with the potentially life-altering implications of cancer.
Dr. Meyer Karre: “Clozapine remains a life-changing treatment for many patients with psychotic disorders resistant to other medications. Non-psychiatrists are often reluctant to prescribe or continue clozapine, related to a poor understanding of risks, including agranulocytosis. Given the frequency of medical comorbidities in patients with psychiatric disorders, it is vital that C-L psychiatrists advocate for best treatment of psychiatric disorders despite possible risks when utilized in the setting of treatment for another medical condition. This case highlights the possibility of safely continuing clozapine with close clinical and laboratory monitoring while undergoing chemotherapy for a co-occurring cancer diagnosis.”
TRANSPLANT PSYCHIATRY AND C-L SUBSPECIALTIES
Death after Psychiatric Contra-Indications to Urgent Liver Transplant following Paracetamol Overdose: an 18-year Cohort Study
Lead presenter: Olivia Impey, MBDhB.

Olivia Impey, MBChB
Paracetamol overdose (POD) is the most common cause of acute severe liver injury (ASLI) in the UK (Kahn, 2010). Without urgent orthotopic liver transplant (OLT), mortality is high. Psychiatric assessment is a crucial part of the work-up. It is time-pressured and often undertaken by C-L psychiatrists without transplant experience. In some cases, assessment identifies absolute psychiatric contraindications (APCIs) precluding transplant in an otherwise medically suitable patient. This study aimed to ascertain how common this is.
Among the 523 patients undergoing assessment for OLT in the study, 102 were in-episode deaths (19.5%). APCIs were identified in 46 patients who were otherwise medically suitable for transplant and later died. This figure represents 8.8% of those undergoing assessment and 45% of those who died. Of this subgroup, 27 (59%) were female and the average age was 44.6 years (range 19-72). The most common primary psychiatric diagnosis was Alcohol Dependence Syndrome, found in 67% (n=31).
Previous research in this area is sparse. One study shows that psychiatric comorbidity in patients who receive a liver transplant does not impact short-term outcomes (Simmons, 2019). Another study reports that death from self-harm after OLT for POD-induced ASLI is infrequent (Cooper, 2009), although there is still significant medical morbidity and mortality (Khan, 2010). This is the first UK study to report a rate of transplant declines on psychiatric grounds.

Olivia Impey, MBChB, (right) with co-author Jennifer Baker, MBChB.
Dr. Meyer Karre: “Every year thousands of patients are waitlisted for a liver transplant with a large percentage having one or more psychiatric diagnoses, including substance use disorders. The authors of this abstract discuss concerns regarding the number of patients declined for a transplant due to psychiatric reasons, particularly given the paucity of research outcomes of liver transplantation in those with psychiatric diagnoses. With a limited number of available organs for transplant, it is important that C-L psychiatrists are educated on the transplant psychiatric evaluation, including what constitutes a psychiatric contraindication for transplant, and what recommendations can be made to help patients become suitable candidates for transplant.”
QUALITY & SAFETY
Empowering Care: A Holistic Approach to Agitation Management through Education and Collaboration in the Hospital Setting
Lead presenter: Margaret Cinibulk, MD.

Margaret Cinibulk, MD
Assistance with management of agitation is a common psychiatric consultation. A 2012 expert consensus, Project BETA, established a validated treatment algorithm for the management of agitation (Roppolo, 2020). Inappropriate management, including excessive use of physical restraints, can result in significant negative health outcomes. Further, the etiology of agitation is often not treated pharmacologically. Studies have shown that educational interventions can safely decrease restraint use in nursing facilities (Huizing, 2006). The presenters’ project aims to improve justification/documentation of physical restraint initiation and selection of appropriate pharmacologic treatment of agitation through educational intervention.
Eighty-five resident and attending physicians participated in didactic presentations. Participants included internal medicine hospitalist attendings and internal medicine/psychiatry/neurology residents. Knowledge scores increased, on average, by 19% after the didactic presentation. On preliminary evaluation, a total of 7, 22, and 32 charts were reviewed during pre-, mid-, and post-didactic intervention periods, respectively. Correct documentation/justification of restraint initiation occurred in 57%, 55%, and 56% of charts reviewed, and percentage of appropriate treatment of agitation with medication occurred in 43%, 68%, and 72% of charts reviewed during the pre-, mid-, and post-didactic intervention periods, respectively.
This project exemplifies the importance of the C-L psychiatrist’s role as a liaison. While the rate of appropriate documentation/justification for initiation of restraint orders did not change throughout intervention, there was an increase in appropriate pharmacologic management of agitation. Educating primary teams about appropriate management of agitation is essential to maintaining patient safety.
Dr. Meyer Karre: “With physical assaults on the rise in hospitals, the ability to safely manage agitation has become a focus for many psychiatrists in emergency and inpatient settings—with pharmacologic management preferred over physical restraint. The authors of this project aimed to improve rationale for physical restraint and increase appropriate pharmacologic management through targeted education for resident and attending physicians. It is worthwhile to note that knowledge scores and use of pharmacologic management increased with educational intervention, highlighting the importance of education on agitation management to ensure the safety of both patients and staff.”
Registration for the 2024 Annual Meeting is Open!!
Registration for the ACLP 2024 Annual Meeting: Promoting Whole Health through Innovative and Integrative Approaches to Consultation-Liaison Psychiatry is now open. Register here. And Book your accommodation at the meeting venue here.

