IN THIS ISSUE: President's Message | Stoudemire Award | Visiting Professors | Posters | What's on the Web | A&E Abstracts
Selection from the latest research impacting C-L Psychiatry
Modernizing the Data Infrastructure for Clinical Research to Meet Evolving Demands for Evidence
Authors: Joseph Franklin, PhD, et al.
Abstract: The authors envisage a modernized infrastructure for clinical research centered around:
- Enabling the collection and rigorous evaluation of multiple data sources for the conduct of clinical trials and other types of clinical research.
- Creating the possibility to reuse health data for multiple purposes.
The potential, they say, is to leverage and streamline data collection, and greatly enhance the value of clinical research evidence generated.
“The ways in which we access, acquire, and use data in clinical trials have evolved very little over time, resulting in a fragmented and inefficient system that limits the amount and quality of evidence that can be generated,” say the authors.
Clinical trial design has advanced steadily over several decades. Yet the infrastructure for clinical trial data collection remains expensive and labor-intensive, and limits the amount of evidence that can be collected to inform whether and how interventions work for different patient populations. Meanwhile, there is increasing demand for evidence from randomized clinical trials to inform regulatory decisions, payment decisions, and clinical care.
“Although substantial public and industry investment in advancing electronic health record interoperability, data standardization, and the technology systems used for data capture have resulted in significant progress on various aspects of data generation, there is now a need to combine the results of these efforts and apply them more directly to the clinical trial data infrastructure.”
Describing their vision for a modernized infrastructure, the authors address the need for multidisciplinary collaboration and suggest ways to measure progress toward this goal.
Clinical trials answer critical questions about the effectiveness and safety of interventions, say the authors. Clinical trial design has advanced steadily over several decades and now includes the use of complex elements, such as master protocols, adaptive platform designs, external control arms, participants in multiple countries, and advanced statistical methods. Yet, the infrastructure for clinical trial data collection has evolved very little. “As technology has changed our interactions with data in modern society, opportunities to improve the infrastructure—meaning the ways we access, acquire, and use data in clinical trials—have become more evident.”
Clinical trial data are typically collected in ‘closed systems’, outside normal health data systems. Accordingly, clinical trials routinely use time- and labor-intensive methods to collect data—creating burdens for both clinicians and patients—when such data may already exist in electronic data records or other real-world sources. Moreover, trials generally lack concurrent data from other sources that may yield important insights into a participant’s health, such as data gathered during activities of daily living or comprehensive patient-reported information beyond what can be collected at site visits. Furthermore, clinical trial data typically only capture a snapshot of a participant’s life, omitting important contextual information about the participant, such as social determinants of health and other factors likely to affect engagement, adherence, and retention. “These limitations...have consequences not only for the number of trials and other studies that can be conducted with available resources but, at least as important, have implications for the validity and generalizability of what is found.”
The authors propose the core elements of a modernized infrastructure that would support clinical trials and other types of clinical studies producing evidence about medical interventions. “We emphasize that the key to meeting the increased demand for new types of clinical evidence is to collect and rigorously evaluate multiple data sources from diverse settings in this modernized infrastructure. This integration will help to shift clinical research from single-use, single-purpose data collection to reusable and multipurpose data collection for the range of studies that may be needed, from randomized clinical trials to observational studies.”
The authors detail their proposals, raise ethical and global issues, and discuss three components required to build a modernized infrastructure:
- Metadata as the core of a reusable, multipurpose data for a modernized infrastructure.
- Rethinking the data elements collected.
- Integrating research and care data systems.
Describing components of a multi-disciplinary taskforce to bring about modernisation, and the challenges they will face, the authors envisage a first step of evaluating and tracking policy alignment of the various stakeholders. Second, progress could be measured through public and private investment and collaboration in projects that allow development and testing of the infrastructure’s core capabilities. Lastly, a concerted effort could be made to track the number and types of research questions or studies that could benefit from reusable, multipurpose data which could help inform strategies for both scaling the infrastructure and determining the most appropriate use cases.
Importance: The authors’ vision for a modernized infrastructure holds the potential to leverage and streamline data collection and greatly enhance the value of clinical research evidence generation. But, as they say: “Challenges abound, and multiple stakeholders will be needed to forge a path forward to achieve this goal.”
Availability: Published by JAMA Network.
Proactive Psychiatry: Innovating the Delivery of Consultation-Liaison Services in a Pediatric Hospital
Authors: Elizabeth Schindler, DO, et al.
Abstract: This article was developed as an outgrowth of debate at a two-day JAMA conference in 2023; authors are collaborators on this effort.
The benefits of a proactive C-L Psychiatry service have been well documented in the adult population, including decreased length of stay (LOS), increased satisfaction among physicians, and enhanced collaborative care. However, there is no available research on the effectiveness of this model in pediatric hospitals. This study compared patients aged 5–18 years on a general medical floor receiving a proactive psychiatry consult to concurrent controls receiving no consult and to historical controls receiving traditional reactive consults.
After adjusting for age, sex, race, insurance type, reason for consult, and medical diagnosis, concurrent control patients had 14% (P = 0.295) longer mean LOS than proactive consults, and historical controls had twice (P < 0.001) the mean LOS of those with proactive consults. Response rate for patient satisfaction scores was low, but responses were modestly more favorable among patients who received proactive C-L services. Follow-up surveys were statistically significantly more favorable after a proactive psychiatry consult service was introduced. Concordance of recommendations was higher for proactive consults than concurrent controls for diagnoses and non-medication recommendations.
Studies investigating the relationship between mental health and the pediatric population found that nearly 20% of hospitalizations in freestanding children's hospitals within the US include a mental health diagnosis. Suicide has become the second leading cause of death in children, adolescents, and young adults aged 10–24 years. Children with chronic medical concerns, which often necessitate multiple hospital admissions, are also at increased risk for depression and suicidal ideation. The mental health crisis for children and adolescents was exacerbated by COVID.
Comorbid psychiatric conditions often lead to greater LOS in the hospital, increased hospital costs, and elevated risk for adverse health outcomes. In one study, youth with mental health disorders were more than five times as likely to exhibit nonadherence, which led to increased hospitalization rates. “Psychiatry C-L teams can help to ameliorate the burden placed upon the hospital system by providing care to pediatric patients who struggle with behavioral health concerns and are admitted to the hospital with complex medical conditions,” say the authors. Significantly, hospitalist satisfaction was also analysed and reported.
Importance: The positive impact of a proactive C-L Psychiatry consultation model was observed in a pediatric hospital and was associated with a lower LOS than concurrent controls and historical reactive consults, higher hospitalist satisfaction among paired responses, and greater concordance of diagnoses and other non-medication recommendations.
Availability: Pre-publication in the Journal of the Academy of Consultation-Liaison Psychiatry (JACLP).

Investigating Change in the Ability to Decentre and Depressive Symptomatology over the Course of a Six-Month Mindfulness-Based Intervention in Patients with Persistent Depression
Authors: Jonathan Hamilton, MD, et al.
Abstract: Mindfulness-based interventions (MBIs) for depression use regular mindfulness practice as a means of helping patients build skills that allow them to respond more adaptively to negative mood. Although effects of practice are assumed to accumulate over time, little is known about the trajectories of change in skills and symptoms beyond the duration of standard eight-week interventions.
Forty-four patients with persistent depression were recruited to participate in a six-month blended MBI plus self-reports of depressive symptomatology and their ability to decenter (the core skill cultivated in MBIs) at baseline, mid-intervention, and after the end of the intervention. Thirty-one participants (70%) completed the intervention having engaged in 68.6% of practices on average.
Trajectories of change in decentering and depression were best described by a combination of a constant change component and a limiting factor indicating decreasing rates with higher previous gains. Bivariate analyses showed significant lagged change-to-change coupling linking earlier changes in decentering with later changes in symptoms. The findings suggest that decentering skills increase throughout longer periods of practice and drive changes in symptoms to move patients closer to recovery or remission.
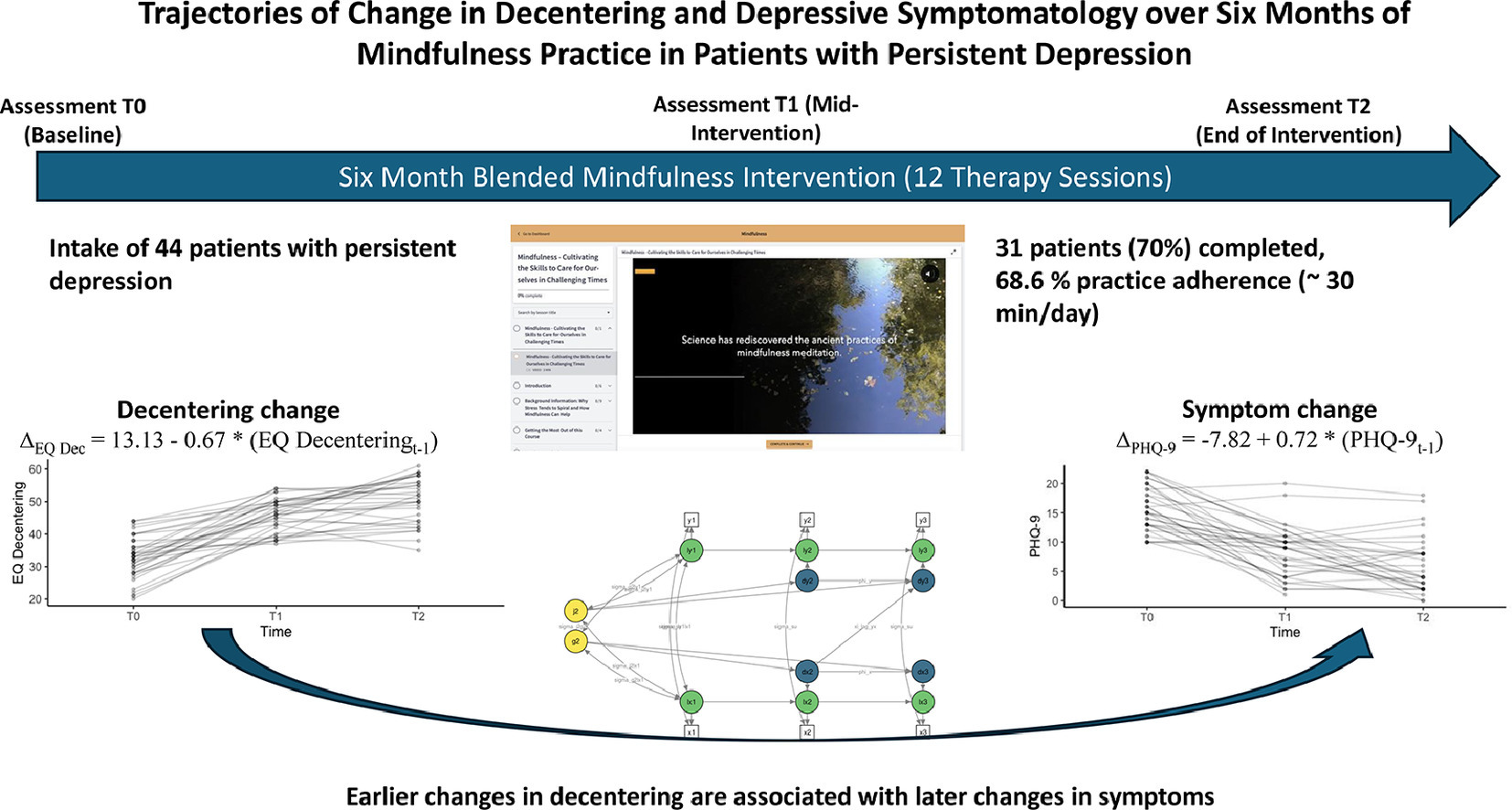
Depression tends to take a course in which symptoms become more persistent, vulnerabilities more engrained, and recurrence increasingly likely. To prevent such courses, it is important to counter vulnerabilities and help patients achieve full and lasting recoveries from episodes. The use of mindfulness training was introduced to the psychological treatment of depression specifically for this purpose and with the intention to provide patients with practices to cultivate portable skills that help them to respond more adaptively to negative mood.
While standard MBIs such as Mindfulness-Based Cognitive Therapy (MBCT) are limited to an eight-week duration, patients are strongly encouraged to continue using the practices and skills they learned beyond the end of the intervention. However, little is currently known about the effects of sustained regular practice and the ways it may impact on the course of the disorder, say the authors. “This is surprising given evidence that lasting effects of MBCT are driven by continued use of practice (Segal et al., 2019) and a considerable body of research with expert meditators that suggests profound cumulative effects of sustained practice (Adluru et al., 2020; Bauer et al., 2019; Chaix et al., 2019; Chételat et al., 2017; Guidotti et al., 2023; Kaliman et al., 2014; Lutz et al., 2004).” The aim of this study was to investigate trajectories of change over a longer period of practice.
Importance: The core skill taught by MBIs is the ability to decenter, that is to ‘step outside of one's immediate experience, thereby changing the very nature of that experience.’ Decentering represents a complex construct that more recently has been described as being subserved by three interrelated metacognitive processes: meta-awareness, disidentification from internal experience, and reduced reactivity to thought content. In line with the early description of decentering by Safran and Segal (1990), who highlighted the importance of experiencing the effects of decentering from the construal of reality as compared to simply acquiring an intellectual understanding, the theoretical rationale guiding the development of MBCT emphasised the need to train the perceptual and cognitive skills that facilitate this process.
In terms of its effects, decentering is assumed to prevent the spiralling of negative thoughts and feelings, with repeated engagement leading to cumulative effects through a number of different pathways. More specifically, Teasdale and colleagues suggested that repeated adoption of a meta-cognitive stance in the face of difficulties would serve to alter tendencies to engage in maladaptive responses to depression, build alternative views of depression, and retrain the very processes that would normally reinforce mutual interactions of negative thinking and underlying schematic models. Sustained mindfulness practice would thus be expected to help patients move towards more complete and lasting recovery.
In a recent study in patients with persistent depression, the authors established the feasibility and acceptability of a blended mindfulness-based intervention that combines online components with brief individual therapist sessions delivered via videoconference to support patients in sustained practice. Completers engaged in an average of 89% of practices, thus showing good levels of adherence across an intervention period of three months. Building on these findings, the current study was designed to investigate the use of this intervention to support patients suffering from persistent depression in their mindfulness practice over six months, with assessments at the beginning, middle, and end of this period.
Availability: Published by Psychiatric Research.
Telehealth Mindfulness-Based Interventions for Chronic Pain, The LAMP Randomized Clinical Trial
Authors: Maria Gonsalves Schimpf, MA, MT-BC, et al.
Authors: Diana Burgess, PhD, et al.
Abstract: How effective are scalable, relatively low-resource mindfulness-based interventions (MBIs) delivered via telehealth for veterans with chronic pain? In this multisite randomized clinical trial, both group and self-paced MBIs improved pain-related function and biopsychosocial outcomes among veterans with chronic pain and high levels of psychiatric comorbidity. The likelihood of 30% improvement from baseline was greater for group MBI at 10 weeks and six months, and for self-paced MBI at 10 weeks, six months, and one year.
Importance These scalable, relatively low-resource MBIs conducted virtually could help accelerate the implementation of nonpharmacological pain treatment in health care systems. Although MBIs are evidence-based treatments for chronic pain and comorbid conditions, implementing them at scale poses many challenges, such as the need for dedicated space and trained instructors.
Chronic pain, a prevalent, debilitating, and costly national problem, disproportionately affects veterans. Guidelines now recommend evidence-based, nonpharmacologic treatment approaches, but they are underused because of myriad barriers at the patient, clinician, and organization levels.
Availability: JAMA Network
Floridas Red Flag Gun Law and Firearm and Nonfirearm Homicide and Suicide Rates
Authors: Catherine Gimbrone, MPH, et al.
Abstract: Firearm homicides are a leading cause of death in the US among individuals younger than 44 years, with over 21,000 deaths from mass shootings between 2014 and 2022. In response to the 2018 Parkland high school shooting that killed 17 people, Florida’s legislature enacted a red flag law permitting the temporary removal of firearms by law enforcement officers from individuals posing a danger to themselves or others. In this paper, the authors estimate the association between Florida’s red flag law enactment and firearm and non-firearm homicide and suicide rates.
Florida’s firearm homicide rate increased from 4.51 deaths per 100,000 population in 2017 to 5.28 in 2021, compared with 4.50 to 6.85 for its synthetic control; Florida’s non-firearm homicide rates decreased slightly from 1.53 to 1.46 compared with 1.56 to 1.49 for its synthetic control. During this period, Florida’s firearm suicide rates increased from 8.21 to 8.85 deaths per 100,000 compared with 8.56 to 9.31 for its synthetic control; non-firearm suicide rates decreased in Florida (7.17 to 6.53) and its synthetic control (7.41 to 7.07).
Importance: Florida is one of the few politically conservative and largely pro-firearm states to pass a law restricting gun ownership. Research into how red flag laws affect firearm-related homicide mortality is scant, with inconclusive findings. However, red flag laws may reduce firearm-related suicide mortality, say the authors.
Availability: JAMA Network